JEFFERSON PARISH, La. — Just like the health care workers at hospitals, the staff members at Louisiana’s nursing homes and adult long-term care facilities have been battling COVID-19 on the front lines, many of them staring down the possibility that the residents they have long cared for are at high risk of serious complications or death if COVID-19 struck.
And just like doctors and nurses at hospitals, those nursing home nurses and aides feared daily they would take the virus home to their families from facilities not fully prepared to handle the invisible enemy.
Many describe having inadequate personal protective equipment, especially as coronavirus was creeping into their facilities, and a shortage of staff that made a tough job grueling.
As WWL-TV revealed in the first of our series Standard of Care, the death toll at metro-area nursing homes continues to climb with more than 20 residents dead from COVID-19 at several facilities.
The death toll is more difficult to track at some adult care facilities, however.
Jefferson Parish Coroner Gerry Cvitanovich said that’s because the deaths are being recorded by home address and some facilities only house patients temporarily.
Oceans Behavioral Hospital is one of those facilities. It’s an in-patient psychiatric treatment hospital, largely for the elderly.
"It could have been avoided in so many ways"
The company has three metro-area locations, in Gretna, Marrero and an 18-bed hospital in Kenner. Patients are transferred in and out of Oceans’ facilities, usually from nursing homes as they need psychiatric care for things like Alzheimer’s Disease, schizophrenia, depression or even addiction.
Sometimes those patients stay for days, some for weeks, some for a few months. The Kenner facility is a small facility as adult care facilities go, but five current and former employees say they think it has some big problems.
“It could have been avoided in so many ways,” said one of the staffers who asked not to be identified for fear of losing a professional license. “These people could probably, possibly still be living if this situation would have been handled a little better, if it would have been handled in a better way.”
Patients like Christopher Miller, 57, were being treated in the 18-bed facility when COVID-19 made its presence known at Oceans. His wife, Cynthia, describes him as a big, strapping guy standing 6 feet 2 inches tall, and she says he loved to eat.


“When I first met him, it was just unbelievable. I've never seen anything like it. And we had gone to Popeye's and he ordered and he said, ‘Give me five piece chicken, fries and a large drink.’ He went on and on. And then he turned to me. He said, ‘What will you have?’ I was like, really,” Cynthia Miller said with a laugh.
They were inseparable until his health caught up with him--diabetes, heart disease--and later, when he was living at Maison Orleans Nursing Home Uptown, gangrene cost Christopher his leg.
“Chris, you wouldn't believe, has come close to death so many times. You know, I thought that he was not gonna make it. He would fight back every time. And we was like, you have 99 lives, you know. I said, then here come this virus and take you out in three days,” Cynthia said.
Christopher was transferred to Oceans from Maison Orleans on March 10.
That was the day before the workers at Oceans say the facility's first confirmed covid-19 patient was sent to the hospital with pneumonia.
But the workers say they did not find out for ten days that they had been treating a COVID-positive patient. They found out after a second patient tested positive and word spread among the nurses.
“Staff members were getting sick and I would think that staff members were getting sick because the lack of PPE and the simple fact that when these patients were sick, we weren't aware,” one worker said.
A spokesperson for Oceans denies staff members weren't told, saying staff members are "always informed" when a patient tests positive for COVID-19.
Insufficient PPE
The staffers we spoke with say Oceans supplied them with surgical masks initially, not N95 masks that offer better protection from the virus, even though some of Oceans’ staff are hands-on with the patients, getting them dressed, helping them to the bathroom, even changing adult diapers. Only after a second patient tested positive were they given N95s they were told to re-use.
By the end of April, they were handed one baggie daily containing a mask, a gown, a face shield and shoe covers to use each shift, an allotment Oceans describes as "adequate."
"Every employee – regardless of their role or location – has had continuous access to an adequate supply of protective gear. Appropriate medical grade masks were made available for every employee since the beginning of the pandemic," the spokesperson said.
Infection control expert and registered nurse Dolly Greene said the surgical masks would be sufficient for most nursing home workers under the CDC’s COVID guidelines or PPE.
The workers were also asked to re-use protective gowns.
“Even if I went in the room with a COVID patient, I knew that I have to keep it, bag it up and save it for the next time, use it again,” a worker said.
In nursing homes or wings of nursing homes housing just COVID-19-infected residents, Greene said, the re-use of gowns could be OK.
“Let's say you've got several rooms and they're all COVID-positive. The gown can be used continuously. Doesn't have to be changed in between," Greene said.
But both she and nursing home expert Charlene Harrington, who has studied nursing homes for 30 years as a professor of Nursing at the University of California at San Francisco, agree those COVID-positive patients should be strictly separated from healthy ones.
And the workers said not all the patients being treated at Oceans Kenner are COVID-positive.
“They certainly should have any infected isolated into a separate unit and not mixed in with other patients,” Harrington said.


Oceans is a one-hallway facility with most of the patient rooms double-occupancy, with doors to them on both sides of the hallway. The workers describe one TV room and one dining room that sick patients and healthy patients were supposed to use at different times. But Harrington says facilities should have common areas for use either COVID-positive patients or healthy patients, not both.
“You need to make these distinctions in where the staff work, where the residents are remain, and you try very hard not to co-mingle. Even Housekeeping can't be in both units. I mean, there are definitive ways in which we're trying to separate and contain,” Greene said.
Fear and Distrust
The workers at Oceans describe a tension-filled work environment that plagued the company long before COVID-19. They say how management handled the staff during the epidemic is a symptom of that.
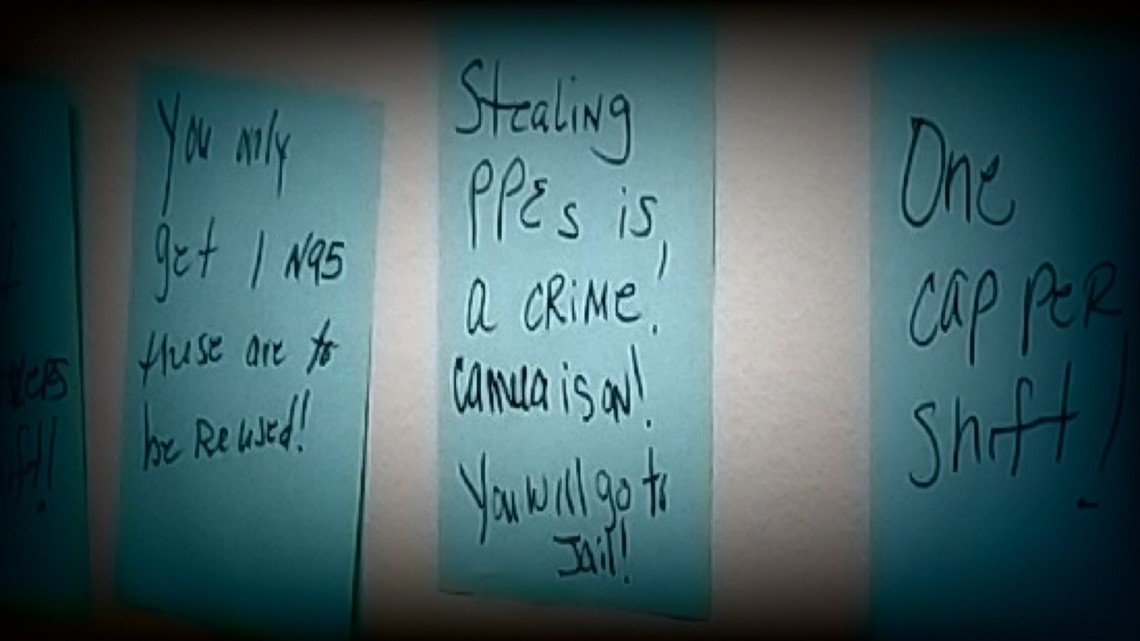
When managers sat out a table of PPE for workers to don every shift in early April, a handwritten sign was posted over it that read, “Stealing PPE is a crime! Camera is on! You will go to jail!"
The workers said fear of the virus and the distrust of management led a number of staffers to refuse to go to work at Oceans early on in the pandemic. Some never went back.

Experts have said that happened at many other long-term care facilities as well.
“It was expressed many of times through our administration that it's like the flu, it's not that serious. And you guys are overreacting,” one worker said.
That view, according to the staffers, led Oceans to handle those COVID patients in a way that they felt put patients and staff at risk.
For example, the workers point to one patient who was sent back to Oceans after a trip to the hospital for pneumonia on March 23. He returned to Oceans before he got his COVID test results back from the hospital. His results would later come back positive.
The workers allege that only half way through his 14-day quarantine, an administrator took the patient out of his in-room isolation, putting him in the only hallway in a wheelchair with no mask on, unprotected.
“He was sitting in the hallway and remember, you're in the area with everybody else. Because the patients walk up and down the hall all day. We have patients who pace all day long. And that's pretty much been in the same area. This was literally one hallway. That's it. That's all it is, is one hallway and a nurse's station,” the worker said.
The Oceans spokesperson calls the allegations made by the staffers false.
"Patients who test positive for COVID-19 are isolated in private rooms away from the general patient population, in accordance with CDC guidelines. At no time are these patients in common areas of the hospital," she said.
“He should have been transferred out"
That's around the same time Christopher Miller, suffering from several chronic health conditions, was being treated at Oceans.
“He should have been transferred out because of his medical history,” the worker said.
Eight days after he first arrived at Oceans, Friday, March 28, he was taken to the hospital with pneumonia. He had COVID-19.
“The doctor called and said, we have to put him on a ventilator because, like he's fighting for his life,” Cynthia Miller recalled.
He had told the staff at Oceans to tell Cynthia he loved her before he was taken to the hospital. After that, Cynthia said he wasn’t able to talk much. That strapping man would be taken down by an invisible virus with no wife, no daughter—who, in Cynthia's words, made him light up like a Christmas tree--by his side.
Making matters worse, when they took Christopher off life support, Cynthia missed the phone call from the doctors. It came in as an 800 number. She thought it was a telemarketer.
The workers said they don't think Christopher Miller had to die if more would have been done to get him out of the facility into a place that the virus had not yet touched.
“We continue to follow our aggressive protocols for prevention, infection control and use of personal protective equipment (PPE) in an effort to limit exposure. We have been working very closely with the Louisiana Department of Health and have been allotted a supply of kits to perform testing in our facility. We are honored to be a part of our state’s response to this public health emergency and to aid other providers in our region,” the spokesperson for Oceans said in a statement in April.
Today, the spokesperson said the three hospital sites had only treated a total of 8 patients, 6 of them in Kenner.
Infection control deficiencies
The Jefferson Parish Coroner said the nature of Oceans’ population makes it difficult to track how many people have died from there. Because patients are not permanent residents, their death records contain the name of their nursing home, not Oceans.
We have heard similar stories about a lack of transparency and staff concerns at several other nursing homes and long-term care facilities. Just like some of the others, Oceans was also cited by the federal agency that oversees Medicare certifications--CMS--for infection control problems last year.
The inspection report says staff failed to properly wash their hands and one aide administered eye drops with gloved hands that had “a hole in the index tip of her left hand.” That citation was marked as "corrected".
Greene and Harrington disagree about whether infection control citations should have been red flags for how adult care facilities would handle the COVID pandemic.
“It's very easy to be given a deficiency because there are so many moving parts to an infection control program,” Greene said, adding that she feels the COVID pandemic is unprecedented with unforeseeable challenges.
Harrington calls the infection control citation "serious."
“It means you haven't developed a plan and implemented a plan that's acceptable to prevent any kind of infection spread. And this virus is so much more virulent. So the main thing is to have enough registered nurses to oversee the infection control and to be able to assess the residents and catch any resident quickly if they develop symptoms and make sure they're isolated and that all the proper procedures are being followed,” Harrington said.
► Get breaking news from your neighborhood delivered directly to you by downloading the new FREE WWL-TV News app now in the IOS App Store or Google Play.

